A groundbreaking clinical trial published in the New England Journal of Medicine (NEJM) has reignited the conversation around how we treat severe, treatment-resistant depression. The study directly compared the effectiveness of IV ketamine infusions with the long-established gold standard: electroconvulsive therapy (ECT).
With 403 participants enrolled, the results challenge long-held assumptions about ECT’s supremacy and elevate ketamine’s role in modern psychiatric care.
Trial Overview
- Study design: Randomized, non-inferiority trial
- Participants: 403 adults with treatment-resistant major depressive disorder (MDD)
- Interventions:
- Ketamine group: IV ketamine administered twice per week for 3 weeks
- ECT group: Standard bilateral ECT administered 2–3 times weekly
- Outcome measures: Depression symptom response rate, cognitive side effects, and adverse events
This head-to-head study was the first of its kind to compare ketamine and ECT in a large, controlled setting. Both treatments have demonstrated high efficacy in the past, but until now, they had never been directly compared on such a scale. The researchers aimed to determine whether ketamine could match the gold standard of ECT not only in efficacy, but in safety and tolerability as well.
Key Findings
1. Comparable Efficacy – With a Twist
- Response rate:
- 55% of patients in the ketamine group responded to treatment
- 41% of patients in the ECT group responded
- Conclusion: Ketamine was non-inferior to ECT in relieving depressive symptoms
- While both treatments were effective, ketamine slightly outperformed ECT in response rate
This finding is especially notable considering ECT’s status as the most effective intervention for treatment-resistant depression. Ketamine’s ability to match—and slightly exceed—ECT’s response rate suggests it may be a viable first-line option for patients who are eligible.
2. Fewer Memory Side Effects
One of the biggest deterrents to ECT is its association with cognitive side effects, particularly memory impairment. Patients often report losing recent memories or experiencing difficulty forming new ones during treatment.
This trial confirmed those concerns:
- Ketamine caused significantly fewer cognitive adverse effects
- Patients receiving ECT reported greater issues with memory loss, confusion, and disorientation
- Patients in the ketamine group maintained better performance on standard cognitive tests over the 3-week treatment window
This advantage gives ketamine a major edge, especially for older adults or individuals whose professions depend on memory and cognitive sharpness.
3. Rapid Relief of Symptoms
Both treatments led to rapid improvements in depressive symptoms. However, ketamine’s onset appeared even faster:
- Participants in the ketamine group reported mood lifts within the first few sessions
- Improvement typically became significant by the end of week two, compared to week three in the ECT group
This rapid effect is a major advantage for patients experiencing severe distress, suicidality, or functional impairment.
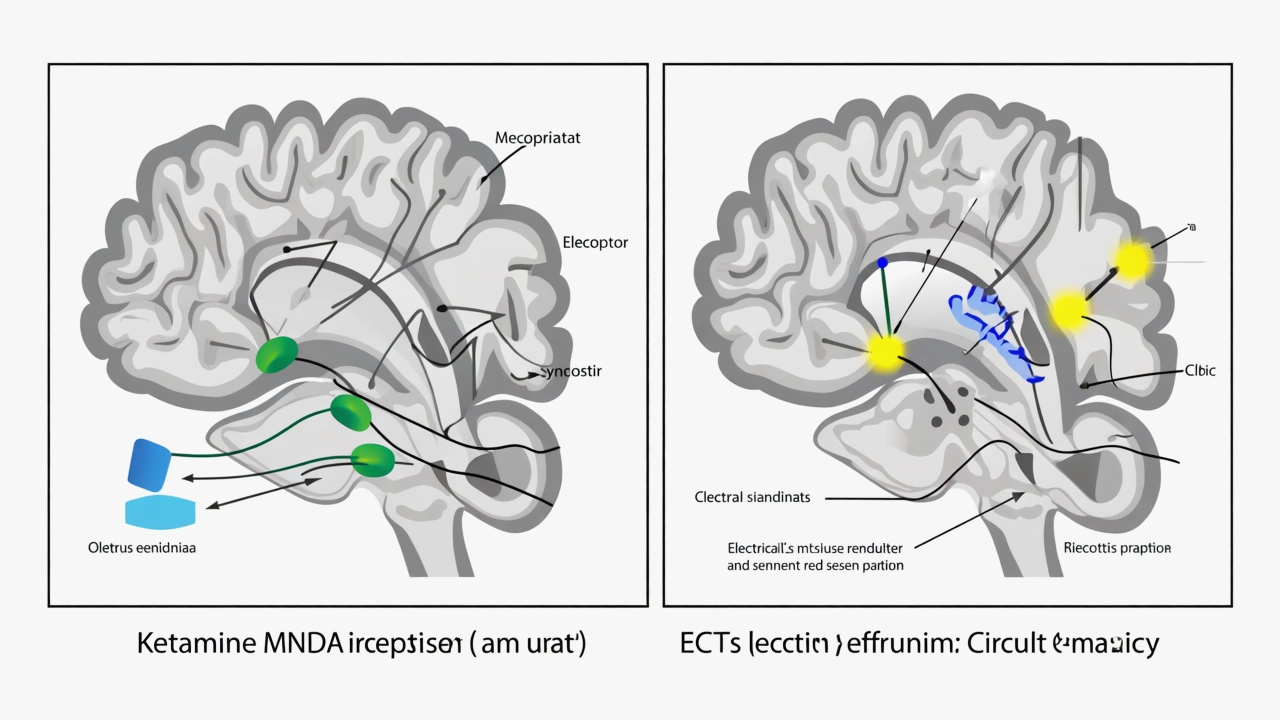
Understanding the Mechanisms
 How Ketamine Works:
How Ketamine Works:
Ketamine operates through a mechanism completely different from traditional antidepressants:
- Glutamate modulation: Ketamine blocks NMDA receptors and enhances AMPA receptor activity, restoring balance in the glutamatergic system.
- Neuroplasticity boost: It promotes the release of BDNF (brain-derived neurotrophic factor), enhancing neuroplasticity.
- Synaptogenesis: Ketamine encourages the formation of new synaptic connections, reversing stress-related damage in the brain.
How ECT Works:
- ECT induces a controlled seizure through electrical stimulation, thought to reset dysfunctional brain circuits.
- It affects neurotransmitter systems and may also stimulate neurogenesis and enhance synaptic plasticity.
While both treatments ultimately enhance brain connectivity, ketamine does so without triggering seizures or requiring general anesthesia.
Broader Clinical Implications
1. Patient Accessibility
ECT is an inpatient or hospital-based procedure requiring anesthesia and monitoring. In contrast:
- IV ketamine can be administered in outpatient clinics
- Sessions are typically 45–60 minutes long, with 15–30 minutes of post-treatment observation
- Less infrastructure is required, expanding availability and access
2. Patient Perception and Acceptance
Many patients are reluctant to pursue ECT due to fear, stigma, or misinformation. Ketamine, on the other hand, carries:
- Less social stigma
- No requirement for sedation or seizure induction
- More autonomy and control for the patient
This makes ketamine more appealing to a broader patient population, particularly those concerned about the invasiveness of ECT.
3. Side Effect Profiles
| Factor | Ketamine | ECT |
| Memory Loss | Minimal, if any | Common, sometimes persistent |
| Sedation Required | No | Yes |
| Time to Recovery | Short | Longer due to anesthesia |
| Risk of Seizures | None | Induced intentionally |
Ketamine’s side effect profile makes it suitable even for individuals with certain comorbidities that may exclude them from ECT candidacy.
Expert Commentary
Dr. Amit Anand, lead author of the NEJM study, emphasized:
“This is the first large head-to-head trial comparing ketamine and ECT. The results show ketamine can be just as effective, with better tolerability and ease of administration.”
Dr. Joan Camprodon, chief of psychiatry at Massachusetts General Hospital, added:
“We are seeing a shift in depression treatment — from decades-old technologies like ECT to fast-acting, neuroplasticity-enhancing agents like ketamine.”
These endorsements underscore the importance of broadening treatment strategies in clinical psychiatry.
Patient Perspectives
Many patients who participated in the trial or have undergone ketamine treatment report profound improvements:
- “I felt like I finally had breathing room — the cloud lifted after the second session.”
- “With ECT, I was scared of losing memories. Ketamine felt gentler but still powerful.”
Patient narratives are increasingly shaping public opinion and influencing mental health care decisions, making ketamine an approachable option.
Watch the Study Breakdown
▶️ A 2-minute visual summary is available here: Watch on YouTube
This short video provides clear, engaging visuals that summarize the study design, findings, and clinical implications.
What’s Next for Research and Practice?
While this trial represents a milestone, more data is needed to answer important questions:
- Long-term outcomes: How do relapse rates compare over 6–12 months?
- Maintenance strategies: What frequency of ketamine infusions sustains remission?
- Psychotherapy integration: Does pairing ketamine with CBT or trauma-focused therapy enhance results?
- Health economics: Will broader ketamine use be cost-effective for healthcare systems?
Ongoing studies are exploring these questions, including trials with oral and intranasal R-ketamine, as well as combination therapy protocols.
Final Thoughts: A Paradigm Shift in Depression Care
The NEJM study is a watershed moment in depression treatment. For decades, ECT stood as the most effective — albeit controversial — last resort. Ketamine now challenges that position, offering a:
- Fast-acting
- Non-invasive
- Well-tolerated alternative
As regulatory frameworks adapt and clinical protocols evolve, IV ketamine is poised to become a first-line option for treatment-resistant depression.
It’s not just a chemical intervention — it’s a new therapeutic philosophy, one that emphasizes neuroplasticity, speed, and patient-centered care.
References
- Anand A, et al. (2023). Ketamine versus ECT in Treatment-Resistant Depression — A Randomized Noninferiority Trial. New England Journal of Medicine.
- Harvard News (2023). Ketamine matches ECT for major depression in large trial. Harvard Gazette.
- YouTube: Ketamine vs. ECT Study Summary
- Wilkinson ST, et al. (2018). Cognitive Effects of Ketamine in Depression: A Systematic Review. Biol Psychiatry Cogn Neurosci Neuroimaging.
McIntyre RS, et al. (2021). Rapid-acting treatments for major depression: an international expert opinion. World J Biol Psychiatry.

 How Ketamine Works:
How Ketamine Works:


